


Hypospadias
Hypospadias is one of the more common congenital malformations of the male genitals.
“Hypo” means “under”, and this typically means that the “urethral orifice”—the hole for peeing—is located lower than usual.
This means that the opening can be...
-
At the head of the penis, but at a lower location (“glanular”)
-
At the area where the head of the penis meets the shaft, or just below (“coronal” or “subcoronal”)
-
Along the shaft (“midshaft”)
-
Or near the scrotum (“penoscrotal”)
-
Or at other locations.
To make things easier to discuss, we can think of the hole as being either “proximal” (closer to the patient’s body) or “distal” (closer to the tip of the penis).
Other findings that come with hypospadias also include a foreskin that doesn’t form all the way around the penis (an "incomplete foreskin"), and a curvature of the penis ("Chordee").
The following are some commonly asked questions about hypospadias.

What causes hypospadias?
There isn’t one single factor that causes hypospadias in all patients. A few factors contribute include:
-
Prematurity
-
A low birth weight
-
Intake of certain hormone-related medications during pregnancy
-
Genetic factors and family history
It is important to remember to not blame either parent for this diagnosis.
How can this problem be corrected?
The first step is for your child to be examined by an experienced hypospadias surgeon.
Medications will not resolve hypospadias.
Surgery for hypospadias can entail a single surgery, or multiple surgeries, depending on the complexity of the case. Hypospadias surgeons often strive for the following:
-
A urethral opening or “pee hole” that is at or near the tip of the penis
-
A relatively straight penis allowing for straight erections
-
A good an unobstructed urine stream
-
An acceptable cosmetic appearance
As a general rule, for relatively straight hypospadiac penises with an opening near the tip, surgery may be done in a single stage.
For proximal hypospadias, severe curvature, or other associated anomalies, there may be multiple stages or separate surgeries involved.
We often tell parents and patients that the best way to decide if there will be multiple stages is often to examine the patient under anesthesia. This means that often, decisions regarding the phases or stages of surgery are made intraoperatively or during surgery.
In general, hypospadias surgeries have the following in common:
-
The need for antibiotic before surgery
-
After surgery, the need for a urinary catheter to stay in the bladder (“indwelling catheter”) for urinary drainage for a certain time period.
-
The need for pain medications after surgery
-
After the catheter is removed, the need to ensure that the child is peeing well with a wide open urethral opening
Who does the surgery for hypospadias?
Pediatric urologists, pediatric surgeons, and select plastic surgeons may all manage hypospadias.
It is very important for a child undergoing hypospadias surgery to have urology follow-up to watch out for functional consequences of repair.
Can I get my child circumcised?
Most hypospadias surgeries result in a “circumcised” appearance. In some countries, differences in societal norms and values can mean that surgeons may try to “preserve” the foreskin when they correct hypospadias.
In the Philippines and in many other countries, the foreskin is used to reconstruct the penis and the urethra. This is why children with hypospadias are often advised to not undergo circumcision without consultation with a pediatric urologist or pediatric surgeon first.
Does my child need surgery for hypospadias?
This is one of the most important (and controversial) questions parents ask when their child has hypospadias.
Unfortunately, there is no easy answer.
The primary goals of surgery for hypospadias are usually to help affected children to be able to pee standing up if they should want to, and to enable them to produce a pregnancy in the future.
This means that some patients with a “distal” hypospadias, or an opening almost at the tip, who can pee standing up and who will still be able to produce pregnancies through normal intercourse ejaculation, may not always “need” surgery.
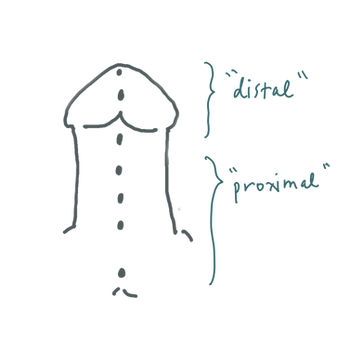
This also means that patients with a “proximal” hypospadias, with an opening far from the tip, or patients with a very severe downward curvature, are often advised to have surgery, since they would usually have difficulty peeing standing up or ejaculating from near the tip of the penis.
A secondary goal is also “aesthetic” or cosmetic, since many persons are uncomfortable with the way a hypospadiac penis looks, even though it may function normally. This is still an important goal that should not be dismissed, as it can be tied to societal expectations and self-esteem.
It is important that parents have an open conversation with their pediatric urologist or pediatric surgeon when discussing the question of surgery. Any benefits of surgery should also be balanced with its risks.
What happens if my child doesn’t get surgery?
Boys with hypospadias who are peeing well and who have no other congenital problems can still lead healthy and fulfilling childhoods.
In the absence of other inborn issues, unrepaired hypospadias itself generally does not cause medical issues. Individualized and open decision making is very important.
When should my child get the surgery? Should we get it as soon as he is born?
This is another controversial question.
Strictly speaking, surgery for hypospadias can be done as early as 6 months or as soon as the child can safely tolerate general anesthesia.
The following are some advantages and disadvantages of early and late surgery:

* There is a growing movement to avoid genital surgery before the child can participate in decision-making. While this movement has its roots in concerns related to intersex children, hypospadias surgery in infancy is also questioned as some feel it is sometimes done for “cosmetic” reasons only, and question the boundaries of parental consent.
Ultimately, every child’s anatomy is different, and thus the decision for each family is different. We advise families to take time to consider their values, their child’s condition, resources available, and the commitment to follow-up and management of potential complications.
The information in this infographic is for general information purposes only.
We encourage you to seek an individualized consult for the most appropriate management. You may book an appointment with us or with your preferred pediatric urologist or pediatric surgeon.
Please feel free to send us a message for questions on pediatric urologic health!
